About 10 percent of Americans suffer from diabetes, and about a fourth of them encounter the scourge of diabetic foot ulcers. Despite relatively successful but complex treatment options, these ulcers take a terrible toll - more than 80,000 amputations every year. Such impacts on so many patients energize aspiring physician-engineers like David Sohutskay to be "all-in" on the pursuit of more innovative and effective solutions during his combined MD/PhD studies.
With about one year remaining in his lab and coursework at Purdue's Weldon School of Biomedical Engineering and two additional years ahead at Indiana University School of Medicine, he says he has found excellent mentors and opportunities proving that the Engineering-Medicine Partnership embodies the "all-in" approach. David graduated with an engineering bachelor's degree from The Ohio State University, where he also studied neuroscience. He then decided he had found the right place for his next career steps: a combination of two world-class Indiana schools embracing interdisciplinary collaboration, with "a strong history in innovation" at its engineering research facilities.
His interest in working with patients while also addressing broader needs results in high standards for himself, as well as for others. "I would like to be on the front lines of helping people, to have access to the clinical data and expertise, and then go into the lab and work on things that potentially reach a much larger group of people," David says. At Purdue, he found a lab that matched his broad interests. It has "a fantastic record in tissue engineering, materials, and stem cells," plus leaders with diverse expertise and crucial real-world connections.
His lab director and co-mentor, Sherry Harbin, a professor of biomedical engineering and basic medical sciences, is "just a great scientist; she's very particular about studies and doesn't cut corners." At the same time, "she is very empowering to students and gives you a lot of room to explore your ideas." Sunil Tholpady, MD, PhD his other co-mentor, coordinates the strength of connections with IU School of Medicine. As a plastic surgeon who "actually knowing how it works in the clinic," including surgical procedure and bandaging of wounds, he is invaluable to the team, David says. In addition, a dermatologist "has helped us understand the physiology of the skin and how to apply that to our engineering design."
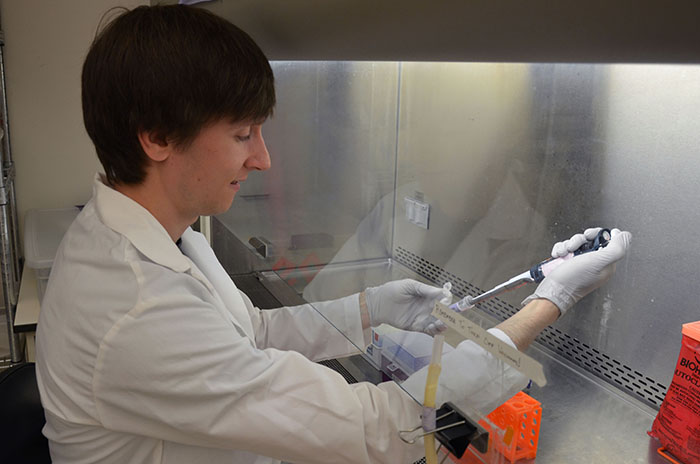
The PhD student's project is to develop a low-cost therapeutic tissue replacement, using different techniques with novel materials researched by Harbin, that can close diabetic foot ulcers rapidly. These ulcers are chronic wounds, related to neuropathy and vascular issues and often slow to heal. The lab uses collagen solutions as part of tissue repairs, advancing clinical translation also valuable in cases other than diabetes. David appreciates the synergy among people, specialties, and institutions. He is lead author for a forthcoming book chapter that will spread knowledge of the "biomechanics and mechanobiology" of collagen.
David's preparation for a career will not be rapid, but it will be well-rounded, with extended learning from a range of people who understand and value the research he is assisting. The preparation is also likely to offer patients great strides for a long time to come, given the prevalence of diabetes and the need for more imaginative engineering in various therapies. The National Institute of Diabetes and Digestive and Kidney Diseases has called tissue repair and regeneration one of the principal future directions for research. It is an area of progress for which an impressive Purdue-IU School of Medicine team will have its clinical skills and wide-ranging imaginations "all-in," thanks to today's collaborative endeavors.